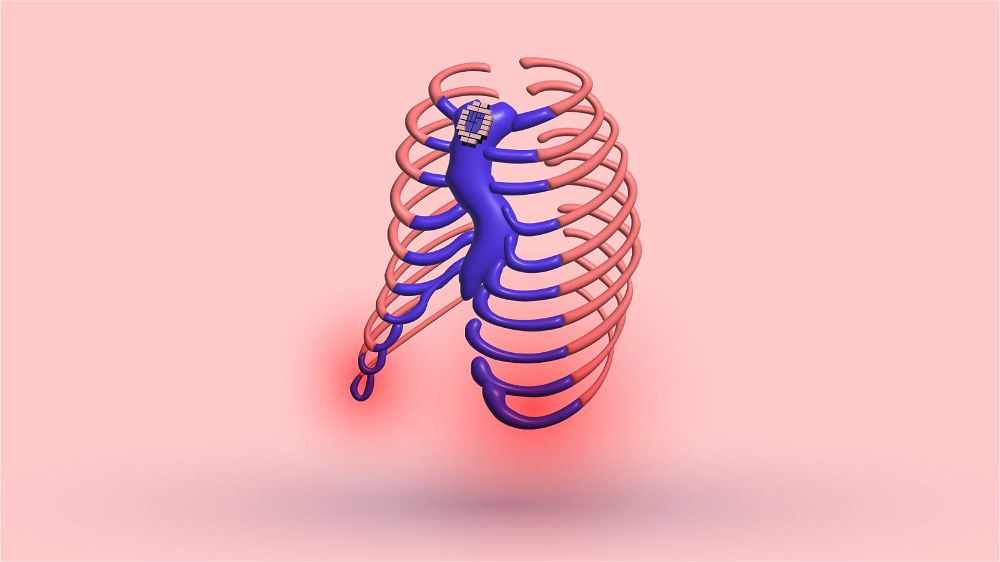
The exact cause of pectus excavatum is still unknown. It probably originates from a genetic defect that results in abnormal musculoskeletal growth.
The cartilaginous part of the rib cage is possibly the primary source of this strange growth pattern.
Rib morphogenesis and development malformations are the most likely causes of pectus excavatum and carinatum.
It is mainly described as genetic, with one’s family history being the leading indicator of risk for deformity. Health professionals and scientists are working hard to find the precise reason for this chest wall deformity.
Studies need to reveal the root cause of the deformity so that researchers can find a cure for future prevention. However, the studies did indicate that other medical conditions are closely related to pectus excavatum.

7 MOST COMMON CAUSES OF PECTUS EXCAVATUM
1. GENETICS

Numerous scientific studies reveal a direct connection between pectus excavatum and genetics.
A study done at the Harvard Medical School by Robert C. Shamberger in 1996 showed that 37% to 47% of all pectus excavatum patients have an affected first-degree relative also suffering from the deformity.
Research on families revealed an inheritance by autosomal dominant, autosomal recessive, X-linked, and multifactorial inheritance in different relatives. So, if your mother and father have a hollow chest, there is a 37% to 47% probability that you’ll also have it.
This study categorizes the pectus excavatum deformity and rib flare posture as primarily genetic.
Another study done in 2012 found plenty of other genetic markers for inverted chest deformities. This study found that roughly 43% of patients with pectus excavatum have a family member with a comparable defect.
In 1934, a student at Ohio State University showed his strange-looking chest. Scientists were interested in it and decided to do an examination. Scientists revealed that eight other members of his family had very similar conditions.
They called this deformity “koilosternia.” This is the same malformation as pectus excavatum. Scientists Snyder and Curtis concluded that this deformity followed an autosomal dominant inheritance pattern.
In 1939, Edmund Stoddard noticed genetic transmission of the deformity in a single family, with 49 cases of pectus excavatum extending over four generations. This researcher also assumed autosomal dominant spreading.
In 2006, researcher HA Creswick issued the first significant family research on pectus excavatum. In this study, researchers investigated 34 families.
Fourteen families displayed the autosomal dominant heritage of pectus excavatum. Four showed autosomal recessive inheritance, and six were X-linked.
Creswick discovered that some cases were inherited through Mendelian genetics. However, most appeared multifactorial. The results of these studies unanimously suggest a genetic cause for pectus excavatum.
2. MARFAN SYNDROME

Research revealed that 70% of patients with Marfan suffer from pectus excavatum. Researchers have reported that these patients experience increased susceptibility to disease and mental anxiety. The sad thing is that it can get worse with age.
Marfan syndrome is a hereditary disorder that acts on the connective tissue. This tissue connects, separates, and supports all other types of tissues in the body. Additionally, it plays a massive part in the proper development and growth of the body.
Around 1 in 5000, people suffer from Marfan syndrome. It is an inherited mutation that impacts males and females from all racial and ethnic groups.
Statistics show that around 3 out of 4 people with Marfan syndrome have inherited it. Usually, it is transferred to the children of a parent who suffers from it.
The main characteristics of Marfan Syndrome are complications in the joints, bones, and ligaments.
If you have pectus excavatum and suffer from pain in these areas, it is critically important to consult your doctor. Along with that, the bones may be longer than usual. Generally, the ligaments are becoming stretchy – like a rubber band.
These patients can also have other skeletal abnormalities that an orthopedic specialist should examine. Because the bones can grow extra long, pectus excavatum and carinatum are more likely to occur.
It is crucial for patients with Marfan syndrome to receive an early and precise diagnosis. Without a prompt diagnosis, the resulting health complications can be deadly.
Receiving early treatment is critically important if you have Marfan syndrome. The pectus excavatum deformity in these patients can be fixed by surgical and non-surgical treatment.
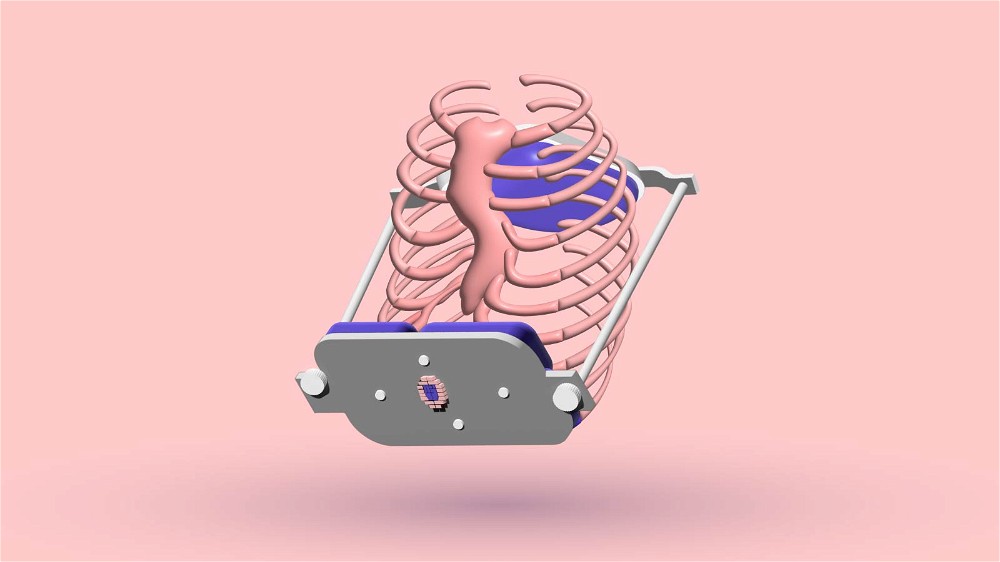
However, connective tissue sickness makes the chest wall bone structure flexible. There is a higher chance of sunken chest re-occurrence after a surgical procedure.
Because of this, the Nuss bar should stay underneath the sternum for a prolonged time. Studies suggest that surgical correction should be postponed until skeletal maturity is reached.
I will cover this entire topic in a chapter dedicated to pectus excavatum in people with Marfan syndrome.
3. SPINAL MUSCULAR ATROPHY
Spinal muscular atrophy (SMA) is a combination of neuromuscular diseases that lead to the loss of motor neurons and the gradual weakening of the muscles. SMA is divided into five categories, depending on the severity.
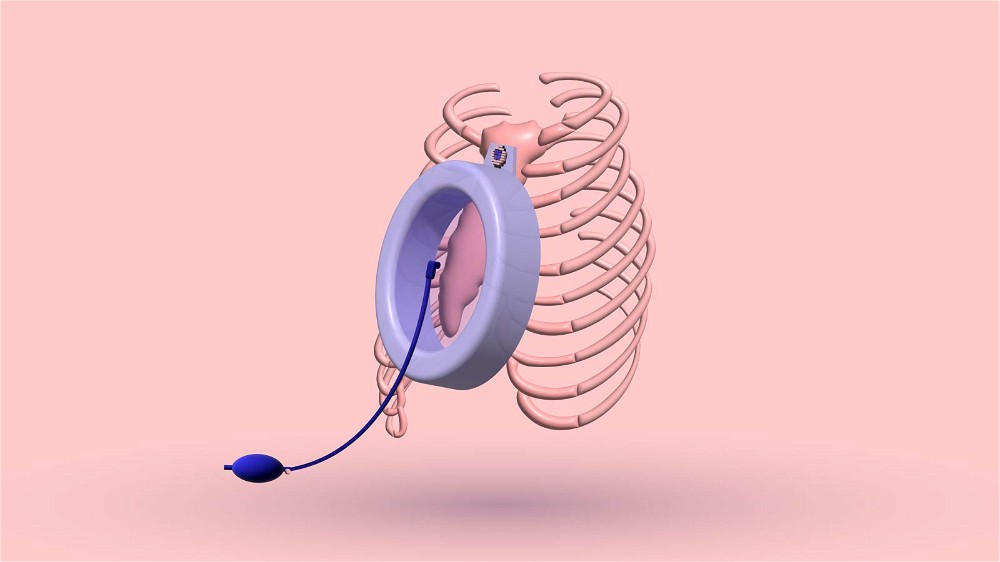
All Spinal Muscular Atrophy (SMA) type 1 patient and those with SMA type 2 with paradoxical respiration can develop pectus excavatum if left untreated.
This is caused by the action of the diaphragm that is not regulated by the intercostal muscles.
As the diaphragm contracts, the stomach expands. The “Bucket handle” action of its insertion on the lower ribs creates an external expansion. This causes the upper chest to sink in.
The result is a sunken chest with the xiphoid process retracted and difficulty developing the lungs. Patients with Spinal Muscular Atrophy type 2 retain the capacity to sit unsupported for a limited period.
However, they can develop breathing failure during their childhood. If left untreated, this can lessen life expectancy and cause problems in later life. SMA Type I and II patients have the highest chance of having pectus excavatum.
Patients with SMA type 3 can walk. They hardly ever have difficulty with breathing or pectus excavatum.
To improve the deformity and stimulate natural lung growth and normal chest wall development, a high-span positive inspiratory pressure and positive end-expiratory pressure (PIP+PEEP) are used.
After successfully establishing high-span PIP+PEEP, pectus excavatum improves in SMA patients. Also, the lungs and chest wall start to grow ordinarily.
4. NOONAN SYNDROME

Sternal abnormalities in patients with Noonan syndrome are present in about 75% to 90% of all sufferers. They either have pectus excavatum or pectus carinatum. Also, the majority of these patients have scoliosis.
Noonan syndrome is a genetic disorder that influences many areas of the body. It manifests with skeletal abnormalities, atypical facial features, small stature, heart problems, and bleeding.
5. LOEYS-DIETZ SYNDROME

Like Marfan syndrome, Loeys-Dietz syndrome affects the connective tissue in many body parts. The connective tissue gives strength and flexibility to the bones, ligaments, blood vessels, and muscles.
Sternal abnormalities are very typical in connective tissue disorders. This is the second most common connective tissue syndrome that causes pectus excavatum.
Depending on the severity, the Loeys-Dietz syndrome is categorized into five types, from Type I to V.
Patients with Loeyz-Dietz syndrome have detectable musculoskeletal problems. They either have an inverted chest (pectus excavatum) or a chest that sticks out (pectus carinatum).
They also have craniosynostosis, scoliosis, kyphosis, a foot that turns inward and upward, flat feet, and lengthened arms and legs with joint deformities.
6. EHLERS–DANLOS SYNDROME

Science has proven a direct correlation between EDS and pectus excavatum. Ehlers-Danlos syndrome is a set of illnesses that upset the connective tissue of the sufferer.
It is inherited and frequently linked to pectus excavatum. It also affects the skin, bones, blood vessels, and other vital organs and tissues.
All flaws in the connective tissue cause severe symptoms of similar conditions. The signs of EDS can range from slightly wobbly joints to life-endangering difficulties.
An extraordinarily high range of joint motion (hypermobility) is present in all patients suffering from this syndrome. Kids and babies with hypermobility typically have weak musculature.
This stops them from developing fundamental motor skills such as walking, sitting, and standing. Their joints are usually loose, unstable, and prone to dislocation and lasting agony.
Babies suffering from this syndrome typically have dislocated hips at birth. Scientific research unveiled that the minimally invasive Nuss procedure gives high functional and beautifying results in patients with Ehlers-Danlos syndrome.
There are strong indications that pectus excavatum correctional surgery is harmless and efficient in EDS patients.
The success rate of caved-in chest operations in patients with connective tissue disorders is the same as in people without these illnesses.
However, the Nuss bar dislocation chance is insignificantly higher in patients with connective tissue disorders.
Even though the Nuss procedure with costal cartilage chondrotomy resulted in notable cosmetic improvements for patients with unequal pectus excavatum, surgeons should be alert to the possibility of continual pleural effusion after the procedure for patients with EDS.
7. CELIAC DISEASE

Pectus excavatum occurs in about 1% of people diagnosed with a Celiac illness. As of 2022, the causes remain unknown. Celiac disease is an immune system illness.
It prevents patients from eating gluten because it will hurt their small intestines. Suppose you’re suffering from this disease and you consume foods that contain gluten.
In that case, your immune system will respond, harming your small intestine. This disease is inherited. It affects every sufferer slightly differently.
Most signs appear in the digestive system or other areas of the body. Also, it cannot be comforting. Some patients suffer from depression, while others only feel abdomen pain and diarrhea.
Some people won’t feel any symptoms at all. The best treatment for Celiac disease is to consume gluten-free food.
CONCLUSION
You don’t have any control over whether you’ll be born with pectus excavatum. As you can see, the pectus excavatum cause is primarily genetic.
Other reasons are the consequences of rare diseases. Usually, people with these rare diseases have more significant concerns than pectus excavatum.
You should even feel grateful that your indented chest deformity is genetic. If your deformity is inherited, please accept your body as it is.
Every single person on this planet is insecure about something. Even some of the biggest adult Hollywood movie stars lack confidence.
Learn to love yourself. As cliché as it sounds, it could’ve been worse.
16 Sources
- Pectus Excavatum Clinical Presentation: History, Physical Examination [Internet]. [cited 2022 Nov 23]. Available from: https://emedicine.medscape.com/article/1004953-clinical#b5
- Shamberger RC. Congenital chest wall deformities. Current Problems in Surgery. 1996 Jun 1;33(6):469–542.
- Brochhausen C, Turial S, Müller FKP, Schmitt VH, Coerdt W, Wihlm JM, et al. Pectus excavatum: history, hypotheses and treatment options. Interactive Cardiovascular and Thoracic Surgery. 2012 Jun;14(6):801.
- Ochsner A, DeBakey M. CHŌNĒ-CHONDROSTERNON: Report of a Case and Review of the Literature. Journal of Thoracic Surgery. 1939 Jun 1;8(5):469–511.
- THE INHERITANCE OF “HOLLOW CHEST” | Journal of Heredity | Oxford Academic [Internet]. [cited 2022 Nov 24]. Available from: https://academic.oup.com/jhered/article-abstract/30/4/139/835809
54 - Marfan Syndrome [Internet]. Marfan Foundation. [cited 2022 Dec 6]. Available from: https://marfan.org/conditions/marfan-syndrome/
- Marfan syndrome - Symptoms and causes - Mayo Clinic [Internet]. [cited
2022 Dec 6]. Available from: https://www.mayoclinic.org/diseases-conditions/marfan-syndrome/symptoms-causes/syc-20350782 - Vorgias D, Bernstein B. Fetal Alcohol Syndrome. In: StatPearls [Internet].
Treasure Island (FL): StatPearls Publishing; 2022 [cited 2022 Dec 6]. Available
from: http://www.ncbi.nlm.nih.gov/books/NBK448178/ - Famy C, Streissguth AP, Unis AS. Mental Illness in Adults With Fetal Alcohol
Syndrome or Fetal Alcohol Effects. AJP. 1998 Apr;155(4):552–4. - Park ES, Park JH, Rha DW, Park CI, Park CW. Comparison of the Ratio of Upper
to Lower Chest Wall in Children with Spastic Quadriplegic Cerebral Palsy and
Normally Developed Children. Yonsei Med J. 2006 Apr 30;47(2):237–42. - Bach JR, Bianchi C. Prevention of pectus excavatum for children with spinal
muscular atrophy type 1. Am J Phys Med Rehabil. 2003 Oct;82(10):815–9. - Noonan syndrome: MedlinePlus Genetics [Internet]. [cited 2022 Dec 6]. Available from: https://medlineplus.gov/genetics/condition/noonan-syndrome/
- Loeys-Dietz Syndrome: Aortic Enlargement, Symptoms, Treatment [Internet].
MedicineNet. [cited 2022 Dec 6]. Available from: https://www.medicinenet.com/loeys-dietz_syndrome/article.htm - Ehlers-Danlos syndrome: MedlinePlus Genetics [Internet]. [cited 2022 Dec 6].
Available from: https://medlineplus.gov/genetics/condition/ehlers-danlos-syndrome/ - What is Celiac Disease? [Internet]. Celiac Disease Foundation. [cited 2022 Dec
6]. Available from: https://celiac.org/about-celiac-disease/what-is-celiac-disease/ - Coeliac disease - Treatment [Internet]. nhs.uk. 2018 [cited 2022 Dec 6]. Available from: https://www.nhs.uk/conditions/coeliac-disease/treatment/